Nurses need to understand the skin and its functions to identify and manage skin problems. This article, the first in a two-part series, looks at the skin’s structure and key functions. This article comes with a self-assessment enabling you to test your knowledge after reading it
Abstract
Skin diseases affect 20-33% of the population at any one time, and around 54% of the UK population will experience a skin condition in a given year. Nurses observe the skin of their patients daily and it is important they understand the skin so they can recognise problems when they arise. This article, the first in a two-part series on the skin, looks at its structure and function.
Citation: Lawton S (2019) Skin 1: the structure and Nursing Times [online]; 115, 12, 30-33.
Author: Sandra Lawton, Queen’s Nurse and nurse consultant and clinical lead dermatology, The Rotherham NHS Foundation Trust.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
- Assess your knowledge and gain CPD evidence by taking the Nursing Times Self-assessment test
- Read part 2 of this series here
Introduction
Skin diseases affect 20-33% of the UK population at any one time (All Parliamentary Group on Skin, 1997) and surveys suggest around 54% of the UK population will experience a skin condition in a given year (Schofield et al, 2009). Nurses will observe the skin daily while caring for patients and it is important they understand it so they can recognise problems when they arise.
The skin and its appendages (nails, hair and certain glands) form the largest organ in the human body, with a surface area of 2m2 (Hughes, 2001). The skin comprises 15% of the total adult body weight; its thickness ranges from <0.1mm at its thinnest part (eyelids) to 1.5mm at its thickest part (palms of the hands and soles of the feet) (Kolarsick et al, 2011). This article reviews its structure and functions.
Structure of the skin
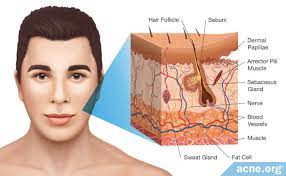
The skin is divided into several layers, as shown in Fig 1. The epidermis is composed mainly of keratinocytes. Beneath the epidermis is the basement membrane (also known as the dermo-epidermal junction); this narrow, multilayered structure anchors the epidermis to the dermis. The layer below the dermis, the hypodermis, consists largely of fat. These structures are described below.
Epidermis
The epidermis is the outer layer of the skin, defined as a stratified squamous epithelium, primarily comprising keratinocytes in progressive stages of differentiation (Amirlak and Shahabi, 2017). Keratinocytes produce the protein keratin and are the major building blocks (cells) of the epidermis. As the epidermis is avascular (contains no blood vessels), it is entirely dependent on the underlying dermis for nutrient delivery and waste disposal through the basement membrane.
The prime function of the epidermis is to act as a physical and biological barrier to the external environment, preventing penetration by irritants and allergens. At the same time, it prevents the loss of water and maintains internal homeostasis (Gawkrodger, 2007; Cork, 1997). The epidermis is composed of layers; most body parts have four layers, but those with the thickest skin have five. The layers are:
- Stratum corneum (horny layer);
- Stratum lucidum (only found in thick skin – that is, the palms of the hands, the soles of the feet and the digits);
- Stratum granulosum (granular layer);
- Stratum spinosum (prickle cell layer);
- Stratum basale (germinative layer).The epidermis also contains other cell structures. Keratinocytes make up around 95% of the epidermal cell population – the others being melanocytes, Langerhans cells and Merkel cells (White and Butcher, 2005).Keratinocytes. Keratinocytes are formed by division in the stratum basale. As they move up through the stratum spinosum and stratum granulosum, they differentiate to form a rigid internal structure of keratin, microfilaments and microtubules (keratinisation). The outer layer of the epidermis, the stratum corneum, is composed of layers of flattened dead cells (corneocytes) that have lost their nucleus. These cells are then shed from the skin (desquamation); this complete process takes approximately 28 days (Fig 3).
Between these corneocytes there is a complex mixture of lipids and proteins (Cork, 1997); these intercellular lipids are broken down by enzymes from keratinocytes to produce a lipid mixture of ceramides (phospholipids), fatty acids and cholesterol. These molecules are arranged in a highly organised fashion, fusing with each other and the corneocytes to form the skin’s lipid barrier against water loss and penetration by allergens and irritants (Holden et al, 2002).
The stratum corneum can be visualised as a brick wall, with the corneocytes forming the bricks and lamellar lipids forming the mortar. As corneocytes contain a water-retaining substance – a natural moisturising factor – they attract and hold water. The high water content of the corneocytes causes them to swell, keeping the stratum corneum pliable and elastic, and preventing the formation of fissures and cracks (Holden et al, 2002; Cork, 1997). This is an important consideration when applying topical medications to the skin. These are absorbed through the epidermal barrier into the underlying tissues and structures (percutaneous absorption) and transferred to the systemic circulation.
The stratum corneum regulates the amount and rate of percutaneous absorption (Rudy and Parham-Vetter, 2003). One of the most important factors affecting this is skin hydration and environmental humidity. In healthy skin with normal hydration, medication can only penetrate the stratum corneum by passing through the tight, relatively dry, lipid barrier between cells. When skin hydration is increased or the normal skin barrier is impaired as a result of skin disease, excoriations, erosions, fissuring or prematurity, percutaneous absorption will be increased (Rudy and Parham-Vetter, 2003).
Melanocytes. Melanocytes are found in the stratum basale and are scattered among the keratinocytes along the basement membrane at a ratio of one melanocyte to 10 basal cells. They produce the pigment melanin, manufactured from tyrosine, which is an amino acid, packaged into cellular vesicles called melanosomes, and transported and delivered into the cytoplasm of the keratinocytes (Graham-Brown and Bourke, 2006). The main function of melanin is to absorb ultraviolet (UV) radiation to protect us from its harmful effects.
Skin colour is determined not by the number of melanocytes, but by the number and size of the melanosomes (Gawkrodger, 2007). It is influenced by several pigments, including melanin, carotene and haemoglobin. Melanin is transferred into the keratinocytes via a melanosome; the colour of the skin therefore depends of the amount of melanin produced by melanocytes in the stratum basale and taken up by keratinocytes.
Melanin occurs in two primary forms:
- Eumelanin – exists as black and brown;
- Pheomelanin – provides a red colour.
Skin colour is also influenced by exposure to UV radiation, genetic factors and hormonal influences (Biga et al, 2019).
Langerhans cells. These are antigen (micro-organisms and foreign proteins)-presenting cells found in the stratum spinosum. They are part of the body’s immune system and are constantly on the lookout for antigens in their surroundings so they can trap them and present them to T-helper lymphocytes, thereby activating an immune response (Graham-Brown and Bourke, 2006; White and Butcher, 2005).
Merkel cells. These cells are only present in very small numbers in the stratum basale. They are closely associated with terminal filaments of cutaneous nerves and seem to have a role in sensation, especially in areas of the body such as palms, soles and genitalia (Gawkrodger, 2007; White and Butcher, 2005).
Basement membrane zone
(dermo-epidermal junction)This is a narrow, undulating, multi-layered structure lying between the epidermis and dermis, which supplies cohesion between the two layers (Amirlak and Shahabi, 2017; Graham-Brown and Bourke, 2006). It is composed of two layers:
- Lamina lucida;
- Lamina densa.
The lamina lucida is the thinner layer and lies directly beneath the stratum basale. The thicker lamina densa is in direct contact with the underlying dermis. It undulates between the dermis and epidermis and is connected via rete ridges called dermal papillas, which contain capillary loops supplying the epidermis with nutrients and oxygen.
This highly irregular junction greatly increases the surface area over which the exchange of oxygen, nutrients and waste products occurs between the dermis and the epidermis (Amirlak and Shahabi, 2017).
Dermis
The dermis forms the inner layer of the skin and is much thicker than the epidermis (1-5mm) (White and Butcher, 2005). Situated between the basement membrane zone and the subcutaneous layer, the primary role of the dermis is to sustain and support the epidermis. The main functions of the dermis are:
- Protection;
- Cushioning the deeper structures from mechanical injury;
- Providing nourishment to the epidermis;
- Playing an important role in wound healing.
The network of interlacing connective tissue, which is its major component, is made up of collagen, in the main, with some elastin. Scattered within the dermis are several specialised cells (mast cells and fibroblasts) and structures (blood vessels, lymphatics, sweat glands and nerves).
The epidermal appendages also lie within the dermis or subcutaneous layers, but connect with the surface of the skin (Graham-Brown and Bourke, 2006).
Layers of dermis. The dermis is made up of two layers:
- The more superficial papillary dermis;
- The deeper reticular dermis.
The papillary dermis is the thinner layer, consisting of loose connective tissue containing capillaries, elastic fibres and some collagen. The reticular dermis consists of a thicker layer of dense connective tissue containing larger blood vessels, closely interlaced elastic fibres and thicker bundles of collagen (White and Butcher, 2005). It also contains fibroblasts, mast cells, nerve endings, functions of the skin lymphatics and epidermal appendages. Surrounding these structures is a viscous gel that:
- Allows nutrients, hormones and waste products to pass through the dermis;
- Provides lubrication between the collagen and elastic fibre networks;
- Gives bulk, allowing the dermis to act as a shock absorber (Hunter et al, 2003).
Specialised dermal cells and structures. The fibroblast is the major cell type of the dermis and its main function is to synthesise collagen, elastin and the viscous gel within the dermis. Collagen functions of the skin– which gives the skin its toughness and strength – makes up 70% of the dermis and is continually broken down and replaced; elastin fibres give the skin its elasticity (Gawkrodger, 2007). However both are affected by increasing age and exposure to UV radiation, which results in sagging and stretching of the skin as the person gets older and/or is exposed to greater amounts of UV radiation (White and Butcher, 2005).
Mast cells contain granules of vasoactive chemicals (the main one being histamine). They are involved in moderating immune and inflammatory responses in the skin (Graham-Brown and Bourke, 2006).
Blood vessels in the dermis form a complex network and play an important part in thermoregulation. These vessels can be divided into two distinct networks:
- Superficial plexus – made up of interconnecting arterioles and venules lying close to the epidermal border, and wrapping around the structures of the dermis, the superficial plexus supplies oxygen and nutrients to the cells;
- Deep plexus – found deeper at the border with the subcutaneous layer, its vessels are more substantial than those in the superficial plexus and connect vertically to the superficial plexus (White and Butcher, 2005).
The lymphatic drainage of the skin is important, the main function being to conserve plasma proteins and scavenge foreign material, antigenic substances and bacteria (Amirlak and Shahabi, 2017).
About 1 million nerve fibres serve the skin – sensory perception serves a critically important protective and social/sexual function. functions of the skin Free sensory nerve endings are found in the dermis as well as the epidermis (Merkel cells) and detect pain, itch and temperature. There are also specialised receptors – Pacinian corpuscles – that detect pressure and vibration; and Meissner’s corpuscles, which are touch-sensitive.
The autonomic nerves supply the blood vessels and sweat glands and arrector pili muscles (attached to the hair) (Gawkrodger, 2007).
Hypodermis
The hypodermis is the subcutaneous layer lying below the dermis; it consists largely of fat. It provides the main structural support for the skin, as well as insulating the body from cold and aiding shock absorption. It is interlaced with blood vessels and nerves.
Functions of the skin
The skin has three main functions:
- Protection;
- Thermoregulation;
- Sensation.
Within this, it performs several important and vital physiological functions, as outlined below (Graham-Brown and Bourke, 2006).
Protection
The skin acts as a protective barrier from:
- Mechanical, thermal and other physical injury;
- Harmful agents;
- Excessive loss of moisture and protein;
- Harmful effects of UV radiation.
Thermoregulation
One of the skin’s important functions is to protect the body from cold or heat, and maintain a constant core temperature. This is achieved by alterations to the blood flow through the cutaneous vascular bed. During warm periods, functions of the skin the vessels dilate, the skin reddens and beads of sweat form on the surface (vasodilatation = more blood flow = greater direct heat loss). In cold periods, the blood vessels constrict, preventing heat from escaping (vasoconstriction = less blood flow = reduced heat loss). The secretion and evaporation of sweat from the surface of the skin also helps to cool the body.
Sensation
Skin is the ‘sense-of-touch’ organ that triggers a response if we touch or feel something, including things that may cause pain. This is important for patients with a skin condition, as pain and itching can be extreme for many and cause great distress. Also touch is important for many patients who feel isolated by their skin as a result of colour, disease or the perceptions of others as many experience the fact that they are seen as dirty or contagious and should not be touched.
Immunological surveillance
The skin is an important immunological organ, made up of key structures and cells. Depending on the immunological response, functions of the skin a variety of cells and chemical messengers (cytokines) are involved. These specialised cells and their functions will be covered later.
Biochemical functions
The skin is involved in several biochemical processes. functions of the skin In the presence of sunlight, a form of vitamin D called cholecalciferol is synthesised from a derivative of the steroid cholesterol in the skin. The liver converts cholecalciferol to calcidiol, which is then converted to calcitriol (the active chemical form of the vitamin) in the kidneys. Vitamin D is essential for the normal absorption of calcium and phosphorous, which are required for healthy bones (Biga et al, 2019). The skin also contains receptors for other steroid hormones (oestrogens, progestogens and glucocorticoids) and for vitamin A.
Social and sexual function
How an individual is perceived by others is important. People make judgements based on what they see and may form their first impression of someone based on how that person looks. Throughout history, people have been judged because of their skin, for example, due to its colour or the presence of a skin condition or scarring. Skin conditions are visible – in this skin-, beauty- and image-conscious society, the way patients are accepted by other people is an important consideration for nurses.
Summary
This article gives an overview of the structure and Part 2 will provide an overview of the accessory structures of the skin and their functions.
Key points
- The skin is the largest organ in the human body
- Approximately half of the UK population will experience a skin condition in any given year
- Nurses observe patients’ skin daily, so need to be able to identify problems when they arise
- Key functions of the skin include protection, regulation of body temperature, and sensation
- How others respond to people who have skin conditions is an important consideration for nurses

- Test your knowledge with Nursing Times Self-assessment after reading this article. If you score 80% or more, you will receive a personalised certificate that you can download and store in your NT Portfolio as CPD or revalidation evidence.
- Take the Nursing Times Self-assessment for this article
References
All Parliamentary Group on Skin (1997) An Investigation into the Adequacy of Service Provision and Treatments for Patients with Skin Diseases in the UK.
Amirlak B, Shahabi L (2017) Skin Anatomy.
Biga LM et al (2019) Anatomy and Physiology. The integumentary system 5.1: layers of the skin.
Cork MJ (1997) The importance of skin barrier function. Journal of Dermatological Treatment; 8: Suppl 1, S7-S13.
Gawkrodger DJ (2007) Dermatology: An Illustrated Colour Text. Edinburgh: Churchill Livingstone.
Graham-Brown R, Bourke J (2006) Mosby’s Color Atlas and Text of Dermatology. London: Mosby.
Holden C et al (2002) Advised best practice for the use of emollients in eczema and other dry skin conditions. Journal of Dermatological Treatment; 13: 3, 103-106.
Hughes E (2001) Skin: its structure, function and related pathology. In: Hughes E, Van Onselen J (eds) Dermatology Nursing: A Practical Guide. Edinburgh: Churchill Livingstone.
Hunter J et al (2003) Clinical Dermatology. Oxford: Blackwell Science.
Kolarsick PAJ et al (2011) Anatomy and physiology of the skin. Journal of Dermatology Nurses’ Association; 3: 4, 203-213.
Rudy SJ, Parham-Vetter PC (2003) Percutaneous absorption of topically applied medication. Dermatology Nursing; 15: 2, 145-152.
Schofield J et al (2009) Skin Conditions in the UK: A Health Care Needs Assessment.
White R, Butcher M (2005) The structure and In: White R (ed) Skin Care in Wound Management: Assessment, Prevention and Treatment. Aberdeen: Wounds UK.